What is a PET scan?
Most people don’t know what a PET scan is, and that’s not necessarily a bad thing. PET stands for positron emission tomography, and it’s most often used as a test for those who have cancer, although it has other applications such as evaluating brain disorders and cardiovascular disease.
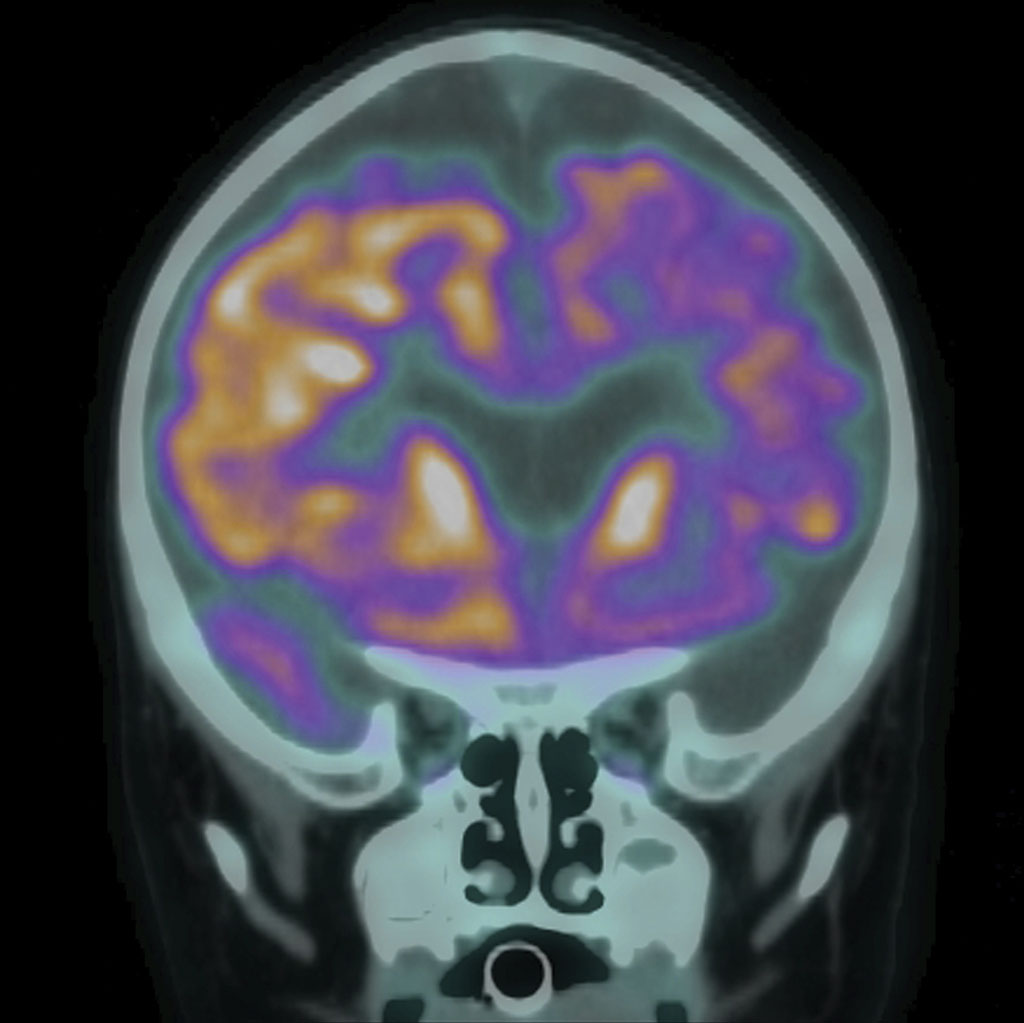
PET is a nuclear medicine imaging test that provides doctors with detailed images of the body’s organs and tissues. Unlike a CT scan, which shows anatomy, a PET scan shows physiology, in the form of increased metabolic activity and blood flow.
Just before having a PET scan, the patient is injected with a radioactive chemical called a radiotracer. Diseased cells within the body absorb more of the radiotracer than healthy cells do. The PET scanner then generates images that identify these concentrations of radiotracer (called “hot spots”), allowing doctors to visualize disease on a metabolic level.
For example, an anatomical test like CT or MRI may reveal a cancerous tumor in an organ such as the lungs. The PET scan will also identify the tumor but can also identify other tumors that the anatomical test may miss (such as metastases). Additionally, by measuring the tumor’s metabolic activity, it can identify more aggressively growing tumors compared to less active ones.
This type of imaging is extremely important to oncologists, because it allows them to actively stage cancers and plan the most effective treatment strategy. In addition to detecting the extent of cancer within the body, PET scanning lets them monitor the effects of treatment and detect early signs of recurrence.
Neurologists may use PET scans to identify specific brain disorders, including epilepsy, dementia, Alzheimer’s disease and brain tumors. It is especially important to distinguish between Alzheimer’s and other forms of dementia, because they are treated and managed very differently.
Cardiologists use PET to assess blood flow to the heart muscle, to assess damage to the heart tissue after a heart attack, detect a buildup of plaque in the coronary arteries or help determine if foreign cells have invaded the heart muscle. They can also help cardiologists predict if a patient may benefit from a surgical procedure, such as coronary artery bypass surgery.
Every radiotracer used in a PET scan is specially made for each patient to target a specific function or tissue in the body. Because it has a short half-life, radiotracers are produced in close proximity to the imaging facility in a special lab that uses a machine called a cyclotron. While the radiotracer is radioactive and exposes the patient to a small amount of radiation, the dose received is the equivalent to what a person would receive spending a year in Denver, Colorado.
PET scanning technology is now commonly incorporated into a hybrid PET/CT scanning machine, where hospitals and imaging centers use both technologies to image the patient both anatomically and metabolically during a single session. This also allows abnormalities like cancer to be closely correlated with anatomy, which helps to ensure treatment is more precise and effective. In fact, the PET/CT scanner was named the medical invention of the year in 2000 by Time Magazine.
Not everyone can have a PET scan. For example, women who are pregnant or are breastfeeding are unable to have a PET scan due to the risks of exposing a fetus to radiation. People with diabetes may not absorb the glucose in the radiotracer, because it can affect scan results. Some people have an allergic reaction to the radiotracer and are unable to have a PET scan as a result. Additionally, those living in rural areas may not have access to a PET scanner in their nearest medical facility, in part due to the high cost of the cyclotrons needed to produce the radiotracers near the PET scanning facility. Traveling to a larger metropolitan area may be required.
Doctors throughout the Bay Area rely on Bay Imaging Consultants to read and interpret PET and PET/CT images to ultimately help them deliver better care to their patients. Several of our radiologists are subspecialty trained in nuclear medicine and PET imaging, which provides an added measure of confidence for those whose lives depend on accurate diagnoses from this potentially life-saving imaging technology.